Wisdom teeth — the third molars that usually appear between the ages of seventeen and twenty-five — are the last teeth to develop. When there is not enough room for them to emerge fully into the mouth, or when they grow at an angle, they are described as impacted. This is a very common finding: many adults have at least one wisdom tooth that has not come through as expected.
This article explains what impacted wisdom teeth are and outlines seven risks that may be associated with leaving a problematic wisdom tooth untreated for too long. It is intended as general information for adults in London who have been experiencing discomfort or who have been told that their wisdom teeth are impacted. It does not replace a clinical examination or personalised advice from a dentist.
What Exactly Are Impacted Wisdom Teeth?
Most people develop four wisdom teeth, one in each corner of the mouth. They typically begin to push through the gum during the late teens or early twenties, although this varies. A wisdom tooth is considered:
- Fully erupted — it has come through the gum completely and sits in line with the other teeth.
- Partially erupted — only part of the tooth is visible above the gum, with the rest still covered by soft tissue or bone.
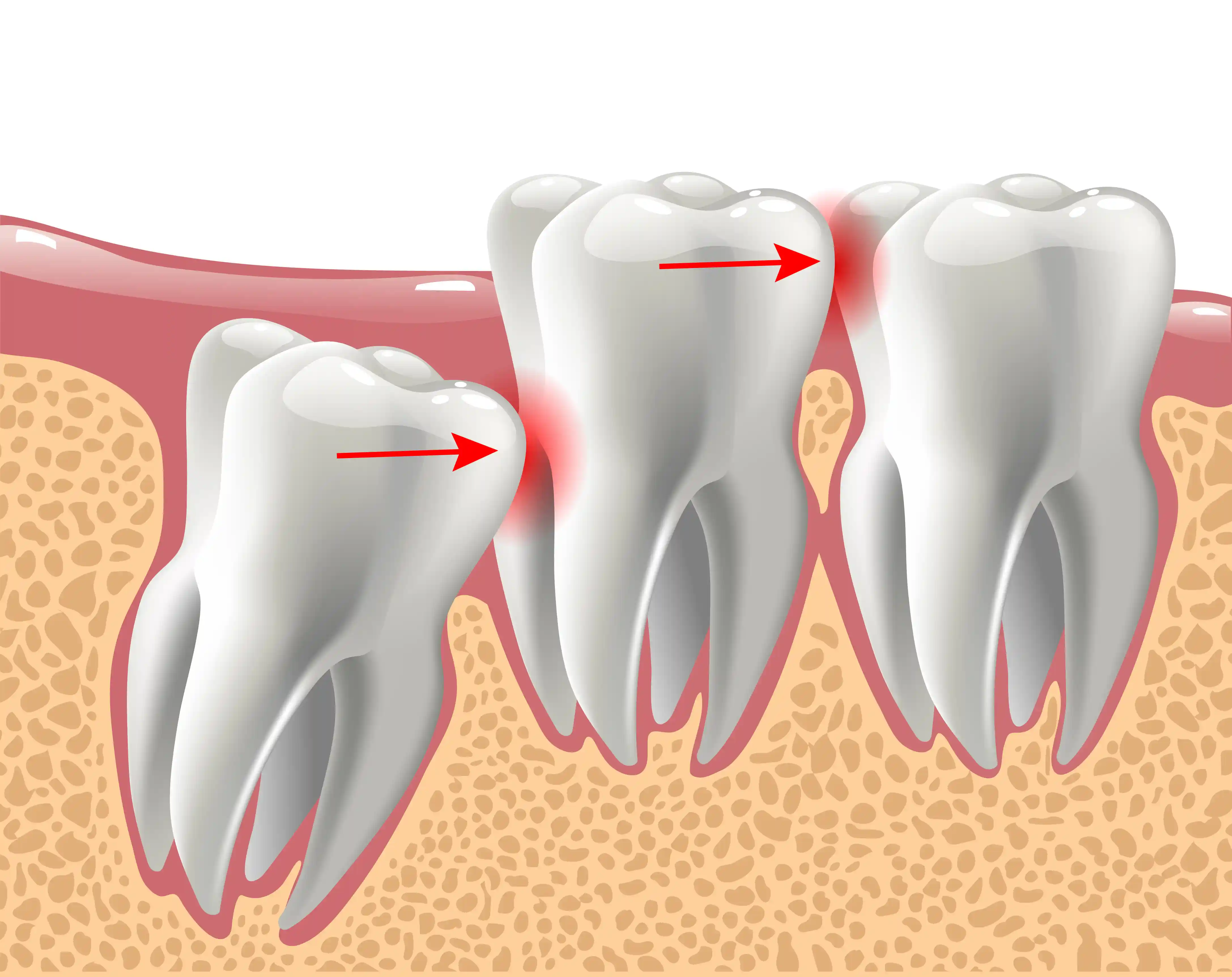
- Impacted — the tooth remains entirely or largely within the jawbone or beneath the gum, often because it is angled against the tooth in front or there is insufficient space for it to emerge.
Signs that may indicate a problem with a wisdom tooth include persistent or recurring discomfort at the back of the mouth, gum swelling or tenderness around the last molar, difficulty opening the mouth fully, food trapping behind the back teeth, ongoing bad breath or a bad taste. It is worth noting that these symptoms can have other causes, so a proper assessment is important before drawing conclusions.
Risk 1 – Repeated Infections and Painful Flare-Ups
When a wisdom tooth is only partially through the gum, a flap of soft tissue often remains over part of the tooth. Food debris and bacteria can become trapped beneath this flap, which the toothbrush cannot reach effectively. Over time, this can lead to a localised gum infection known as pericoronitis.
Pericoronitis may cause soreness and swelling around the affected tooth, difficulty chewing or opening the mouth comfortably, a bad taste or unpleasant odour, and, in some cases, swelling that extends into the cheek or jaw area. Mild episodes can sometimes be managed with improved cleaning and a saltwater rinse, but the condition has a tendency to recur. If infections keep returning, a dentist may recommend that the wisdom tooth is removed to reduce the cycle of flare-ups.
It is important to be aware that pericoronitis can occasionally become more serious if left untreated, potentially spreading to surrounding tissues. If you notice worsening swelling, difficulty swallowing, or a raised temperature, seek dental advice promptly.
Risk 2 – Possible Damage to Neighbouring Teeth
An impacted wisdom tooth that presses against the second molar — the tooth directly in front of it — can make that area very difficult to clean. Bacteria and plaque may accumulate in the tight space between the two teeth, increasing the risk of decay developing on the neighbouring tooth. In some cases, the pressure from an impacted wisdom tooth can also contribute to root resorption of the adjacent tooth, although this is less common.
This risk varies considerably between patients. The angle and depth of the impacted tooth, the shape of the roots, and the patient's oral hygiene all play a role. A dentist will assess these factors using X-rays and a clinical examination to determine whether the neighbouring tooth is at risk and whether intervention is advisable.
Risk 3 – Cysts and Other Jaw Changes (Uncommon but Important)
Every tooth develops within a small sac of tissue inside the jawbone. In some cases, this sac can fill with fluid and enlarge, forming what is known as a dentigerous cyst. A cyst associated with an impacted wisdom tooth may grow slowly and without obvious symptoms for some time, but if left undetected it can gradually affect the surrounding bone, and in rare cases, nearby teeth or other structures.
It is important to stress that cyst formation is not common. However, it is one of the reasons why dentists may recommend periodic X-rays of impacted wisdom teeth that are being monitored, even if they are not currently causing pain. If a cyst is identified, the dentist will discuss the appropriate course of action, which may include referral for further investigation or treatment.
Risk 4 – Crowding and Unwanted Movement of Teeth
The role of wisdom teeth in causing crowding of the front teeth has been debated within dentistry for many years. Current evidence suggests that wisdom teeth are unlikely to be the sole cause of crowding, which is influenced by a range of factors including jaw growth and natural tooth drift over time. However, an impacted wisdom tooth can contribute to localised crowding at the back of the mouth, making the area more difficult to keep clean and potentially affecting the alignment of neighbouring teeth.
For patients who have previously had orthodontic treatment, the question of whether wisdom teeth could affect the stability of their results is a common concern. While wisdom teeth alone are unlikely to undo the effects of braces or aligners, they can make it harder to maintain alignment in the back of the mouth. If you have concerns about crowded or crooked teeth, it is worth discussing the position of your wisdom teeth with your dentist as part of the broader picture.
Risk 5 – Ongoing Discomfort and Jaw Ache
Some patients experience a persistent, low-level ache or intermittent pain around an impacted wisdom tooth. This may be related to the tooth pressing against bone or adjacent teeth, or to low-grade inflammation in the surrounding gum tissue. In some cases, discomfort around the wisdom teeth may be associated with tension or aching in the jaw, which can affect chewing comfort.
It is important to note that jaw pain and facial discomfort can arise from a number of causes, including temporomandibular joint (TMJ) issues, teeth grinding, and stress-related muscle tension. Not all discomfort at the back of the mouth is caused by wisdom teeth. A thorough clinical assessment is essential to identify the source of the problem before deciding on treatment. Your dentist will examine the area and may take X-rays to build a clear picture of what is contributing to your symptoms.
Risk 6 – Needing Unplanned Treatment at Inconvenient Times
One practical risk of delaying an assessment of impacted wisdom teeth is that symptoms can worsen at short notice. An infection may flare up over a weekend, during a holiday, or in the lead-up to an important event such as a wedding, examination period, or work deadline. Dealing with wisdom tooth pain on an emergency basis is rarely convenient, and the treatment options available in an urgent situation may be more limited than those offered as part of a planned appointment.
There is a clear benefit in discussing your wisdom teeth with a dentist while you are symptom-free or experiencing only mild discomfort. This allows time to take X-rays, consider the options, and — if removal is recommended — plan the procedure at a time that suits your schedule, with appropriate aftercare arrangements in place. Decisions made calmly and with good information tend to lead to a better experience than those made under pressure.
Risk 7 – More Complex Treatment if Problems Progress
In younger adults, the roots of wisdom teeth may not yet be fully formed and the surrounding bone tends to be slightly less dense. These factors can make extraction more straightforward in some cases. As patients get older and roots continue to develop, the tooth may become more firmly anchored in the jaw, and its proximity to important structures — such as the inferior alveolar nerve, which provides sensation to the lower lip and chin — may need to be considered more carefully.
This does not mean that older patients cannot have wisdom teeth removed safely. It does mean that, in some cases, the procedure may be more involved, recovery may take a little longer, and the patient may be referred to an oral surgeon or hospital-based service if the treating dentist considers this appropriate. Each case is assessed individually, and a dentist will always explain the reasoning behind any referral.
How Do I Know if It Might Be Time to Discuss Removal?
Consider arranging an assessment with your dentist if any of the following apply:
- You have experienced repeated episodes of pain, swelling, or infection around a wisdom tooth.
- Your dentist has identified decay, gum disease, or other changes on an X-ray near an impacted wisdom tooth.
- You are finding it difficult to clean the area behind your back molars effectively.
- You have been advised during a routine check-up that your wisdom teeth may need attention.
- You are experiencing unexplained discomfort in the jaw or at the back of the mouth that has not settled with simple measures.
It is equally important to know that not all wisdom teeth need to be removed. If a wisdom tooth is fully erupted, free from decay, in a healthy gum environment, and easy to clean, there may be no clinical reason to extract it. The decision should always be based on a careful assessment of your individual situation, not on a blanket policy.
What to Expect from a Wisdom Tooth Assessment at Our London Practice
If you visit our dental practice in South Kensington with concerns about your wisdom teeth, the appointment will typically involve the following:
- A review of your symptoms and dental history — your dentist will ask about any pain, swelling, or other issues you have noticed, as well as your general dental and medical history.
- A clinical examination — this includes a visual and tactile examination of the wisdom tooth area and the surrounding gum tissue.
- X-rays, where clinically appropriate — a dental X-ray (such as a periapical or panoramic radiograph) helps the dentist to see the position, angle, and root formation of the wisdom tooth, as well as its relationship to neighbouring teeth and other structures.
- A discussion of your options — based on the findings, your dentist will explain whether removal is recommended, whether monitoring is more appropriate, or whether a referral to another service may be advisable. You will have the opportunity to ask questions and take time to consider your options before making a decision.
In some cases — for example, where a wisdom tooth is deeply impacted or in close proximity to the nerve canal — the dentist may recommend referral to an oral surgery service for further assessment or treatment. This is a routine part of safe dental practice and ensures that more complex cases receive the appropriate level of care.
Recovery in Straightforward Cases
For uncomplicated wisdom tooth extractions carried out under local anaesthetic, most patients can expect the following general pattern of recovery:
- First one to two days: some soreness, swelling, and minor bleeding from the extraction site are normal. Swelling tends to peak around the second day.
- Days three to seven: discomfort usually begins to ease, and swelling gradually reduces. Most patients feel significantly better within a week.
- Two weeks and beyond: the socket continues to heal beneath the surface. Full healing of the soft tissue and underlying bone takes several weeks, but day-to-day comfort usually returns well before this.
Your dentist or oral surgeon will provide personalised post-operative instructions following the procedure. General guidance that commonly applies includes avoiding smoking, as this significantly increases the risk of a painful complication known as dry socket; eating soft foods and avoiding very hot drinks for the first day or so; keeping the area clean by gently rinsing with warm salt water from the day after the extraction; and avoiding vigorous exercise for a day or two. It is important to follow the specific advice given to you by your treating clinician, as recommendations may vary depending on the complexity of the extraction and your individual circumstances.
When Waiting and Monitoring May Be Appropriate
Removal is not always the right course of action. There are a number of situations in which a dentist may recommend keeping a wisdom tooth under observation rather than extracting it:
- The tooth has erupted fully and is functioning normally within the bite.
- It is symptom-free and there are no signs of disease on X-ray.
- The patient is able to clean it effectively as part of their daily oral hygiene routine.
- There are medical or personal factors that make a period of monitoring preferable to immediate surgery.
Shared decision-making is a fundamental principle of good dental care. Your dentist will explain the pros and cons of each option and support you in reaching a decision that is right for you. If monitoring is chosen, periodic review — including repeat X-rays at intervals determined by your clinician — helps to ensure that any changes are detected early.
Once any discomfort or functional issues related to your wisdom teeth have been resolved, maintaining the health and appearance of the rest of your smile becomes the focus. For patients interested in improving the shape or edges of teeth with composite bonding, this is something that can be discussed at a routine appointment once healing is complete and your mouth is comfortable.
Next Steps – Arrange a Wisdom Tooth Consultation
If you have been experiencing discomfort around your wisdom teeth, or if you have been told that one or more of your wisdom teeth are impacted, arranging a consultation is a sensible first step. An assessment allows your dentist to examine the area, take any necessary X-rays, and explain your options clearly — with no obligation to proceed with treatment on the day.
At our London practice, we aim to provide straightforward, honest information so that you can make an informed decision about your care. Whether the outcome is a recommendation for removal, a plan for monitoring, or reassurance that no action is needed, the goal is always to ensure you understand your situation and feel comfortable with the next steps.
If you would like to discuss your wisdom teeth, please contact us to arrange a wisdom tooth consultation in London. Our team will be happy to help you find a convenient appointment time.
Cosmetic Dental Team
Cosmetic Dentistry Clinic at Cosmetic Dentistry Clinic
With years of experience in cosmetic and restorative dentistry, Cosmetic is dedicated to helping patients achieve their perfect smile through personalised care and cutting-edge techniques.

